cancer It is transported from one organ to another by invisible bubbles. Understanding these microscopic messengers could transform the fight against metastasis.
Preventing cancer from spreading throughout the body is the goal of our team at the Department of Electrical Engineering at the School of Advanced Technology (ÉTS).
In collaboration with Professor Julia Bernier and biology experts at McGill University Health Center Research Institute, we are working to understand how cancer transforms into metastasis. In other words, how do they invade other organs?
Related: Hidden warning signs discovered in the gut may increase cancer risk
For about 8 years, my team is studying Lipid nanoparticles. They are only 100 nanometers in size and invisible to the naked eye. our first task is to understand Path of metastasis. Next, try to determine different ways to inject drugs into the body.
Lipid nanoparticles, such as liposomes, differ from traditional cancer treatment approaches because they deliver drugs directly to tumor cells. This increases efficacy and reduces toxicity compared to traditional chemotherapy.
Researchers have demonstrated Liposomes target tumors more effectively and reduce side effects. observed by others These nanomedicines have been shown to improve the penetrance and specificity of treatment, especially in the case of metastasis.
These results confirm that nanomedicines can make cancer treatments more targeted, more effective, and improve tolerability.
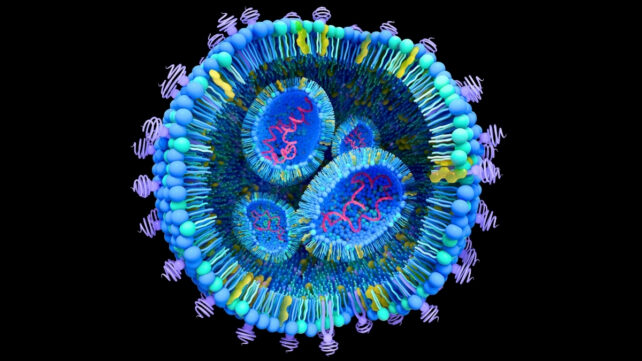 Lipid nanoparticles deliver drugs directly to tumor cells. (Tumeggy/Science Photo Library/Getty Images)
Lipid nanoparticles deliver drugs directly to tumor cells. (Tumeggy/Science Photo Library/Getty Images)
small particles that cause diffusion
All cells in our body, whether healthy or cancerous, release small particles called extracellular vesicles. These tiny bubbles of lipids and proteins also contain genetic information.
When cancer cells release vesicles into the bloodstream and are transferred to healthy cells, their DNA can change and turn them into cancer cells. This causes the cancer to spread to other organs, such as the liver. This mechanism is the basis of metastasis.
The problem is that extracting and studying these natural vesicles is a long and difficult process. To speed up research, my team uses tiny devices called micromixers to produce artificial copies called liposomes.
Our research team creates particles that resemble natural vesicles by mixing different solutions such as lipids, proteins, water, and ethanol. The challenge is understanding which lipids and proteins are included in extracellular vesicles to generate liposomes.
These liposomes are then injected into liver cancer cells to see how they react. The more a cell retains these particles, the better the copy proves to mimic reality.
In a typical experiment, liposomes are manufactured using precise parameters to reproduce the size and charge of extracellular vesicles. It can also be made visible by staining with fluorescent markers.
These liposomes are incubated with cancer cells grown in our laboratory. This makes it possible to image and measure in real time how and at what rate liposomes are absorbed and expressed by cancer cells without affecting the cells.
Our results show that the more similar the size and charge of liposomes to natural vesicles, the more effectively they are absorbed. This allows us to see how their chemical and physical composition affects their uptake into cells, as well as their possible role in tumor development.
Observe the behavior of liposomes
Our goal is to understand how these extracellular vesicles are transported into hepatocytes and cause metastasis. The main challenge is to ensure that these liposomes can mimic extracellular vesicles.
Currently, protein encapsulation efficiency has been achieved at 50%. We aim to increase this to 90%. This is expected to explain how metastases form and make it possible to block them. Once the technology is refined, our team will conduct tests on rats.
In the long term, this research could be a game-changer for many patients by preventing the formation of metastases and increasing their chances of survival. Our goal is to understand and block metastasis.
Towards new treatments
Our team is working not only to understand the process, but also to develop new weapons against cancer. The idea is to use these liposomes as small shuttles that can transport drugs directly into cancer cells.
The diameter of liposomes varies depending on the cancerous organ being treated. Therefore, it is very important to properly characterize and understand the properties of these liposomes.
For example, researchers are currently testing encapsulation of turmeric. Anticancer effects are being studied. Our team is doing the same to observe how cancer cells respond to these liposomes.
Turmeric, and more specifically the curcumin it contains, is thought to help fight cancer by slowing the growth of tumor cells and promoting their destruction in the body.
lots of research It has been shown to have anti-inflammatory and antioxidant properties and can enhance the effectiveness of cancer treatment. Encapsulating turmeric in liposomes increases its ability to reach and target diseased cells.
Unraveling the secrets of the cancer epidemic
In addition to this molecule, other molecules such as paclitaxel are already used in cancer treatment in the form of liposomes. Encapsulated paclitaxel improves drug delivery and tolerance.
There is also an innovative strategy that uses liposomes to transport small pieces of DNA. antibody These act as messengers and help the body better detect and fight diseased cells.
These approaches are examined below. some scientific research They are already used to treat certain cancers, and new advances are made every year to improve their effectiveness and safety.
Related: Scientists use ultrasound to ‘3D print’ materials deep inside the body
By using liposomes to replicate the body’s natural vesicles released by cancer cells, our team hopes to unlock the secrets of how cancer spreads and determine effective approaches to stopping it. Our research paves the way for more targeted treatments that prevent metastasis and improve patient survival.![]()
Vahe Nergizianprofessor title, Higher Technical School (ÉTS)
This article is republished from conversation Under Creative Commons License. please read original article.
